What is Sleep Apnea?
Sleep Apnea is a sleep-related breathing disorder that damages your health, family relations, working performance and social lives.
The most obvious symptom of Sleep Apnea is loud snoring. Estimated 80% of sleep apnea sufferers are unaware that they suffer from OSA, and therefore are untreated.
Sleep Apnea is one of the most common kinds of sleep disorders. People suffering from Sleep Apnea would have their airway being blocked, and stop breathing during sleep. Such events can happen hundreds of times during sleep and each event may last for a few seconds to a few minutes. This causes lowering of oxygen saturation in blood, frequent awakenings and poor sleep quality.
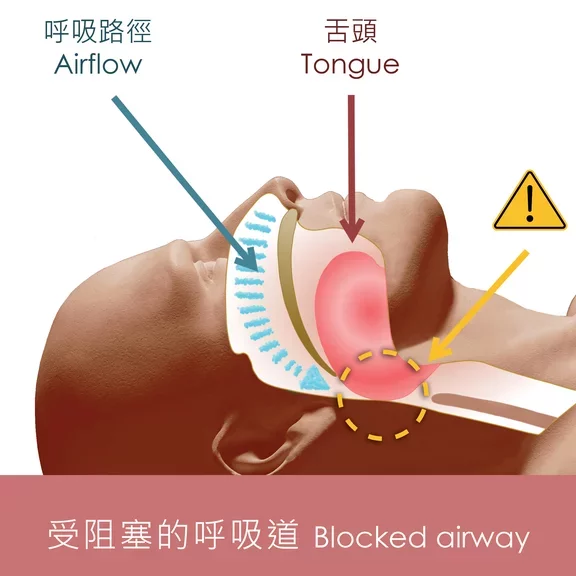
Obstructive sleep apnea (OSA) – During normal breathing, the airway is clear and open, allowing air to flow freely in and out of the lungs. OSA is the most common type of sleep apnea. It occurs when tissues in the throat collapse and block the air flow in and out of the lungs during sleep.
Central sleep apnea (CSA) – which is not as common as OSA – where the brain or nerves fail to signal the muscles that control breathing to tell them that you need to take a breath
Mixed sleep apnea (MSA) – where obstructive and central sleep apnea occur together
The AHI is calculated by dividing the number of apnea events by the number of hours of sleep. The AHI values are categorized as:
|
Level of Severity
|
AHI
|
|
Normal |
<5 /hour |
| Mild | 5-15 /hour |
| Moderate | 16-30 /hour |
| Severe | >30 /hour |
More about OSA (Obstructive sleep apnea)
Obstructive Sleep Apnea (OSA) is a breathing problem that occurs when we sleep. The upper airway keeps blocking, partially or totally, because the tongue and upper muscles in the throat relax, causing an obstruction in breathing (apnea) lasting over 10 seconds. This obstruction or pause in breathing occurs repeatedly throughout the night. The pauses are followed by gasping, snoring and/or restlessness.
During normal sleep, the muscles that control your tongue and soft palate hold the airway open. If these muscles relax, your airway will become narrower and the soft or floppy part of the throat vibrates; the noise of snoring results. If your throat is already narrow, or the muscles relax too much, your airway can become completely blocked, which prevents breathing.
Explore more
Why do we snore?
It is a matter of poor “plumbing”. Our anatomical make-up or obstacles in the throat can inhibit the flow of air and make a noise, what we called "Snore".
There is a clear hereditary aspect, and other factors such as obesity, smoking, drinking, certain drugs or just extreme tiredness can all contribute to snoring. Finally, we are more likely to snore if we sleep on our back.
Snoring may be a sign of sleep apnea, but only specialised doctors are qualified to draw any conclusions. CPAP treatment usually cures snoring.
What are the characteristics of high risk group?
1. Male
Men are 2 to 3 times more likely to have sleep apnea than are women. However, women increase their risk if they're overweight or if they've gone through menopause.
2. Obesity
More than half of people with obstructive sleep apnea are either overweight (body mass index, or BMI, of 25-29.9) or obese (BMI of 30.0 or above). A 10% weight gain raises your risk of OSA by six times
3. Neck circumference is above average
Men with a neck circumference above 17 inches and women with a neck circumference above 15 inches have an increased risk of developing or having obstructive sleep apnea.
4. Short chin
Short chin increases the risk of obstructive sleep apnea, the small lower jaw may not allow enough room for the tongue, which can fall to the back of the throat and block the airway during sleep.
5. Irregular thyroid gland excretion
Studies indicated that obstructive sleep apnea can increase the prevalence of hypothyroidism and also hypothyroidism can increase the prevalence of obstructive sleep apnea.
6. Curved nasal septum / Displaced nasal bones
A deviated septum can block the airflow through your nasal passages, resulting in snoring and sleep apnea.
7. Suffering from endocrine diseases
Endocrine diseases can contribute to or worsen the symptoms of sleep apnea, while treatment can help relieve them. The interactions between sleep-disordered breathing and hormones are complicated, they can have a cyclical effect on each other.
8. Alcoholic or Smoking
Smoking and higher alcohol intake are causally associated with an increased risk of obstructive sleep apnea.
9. Taking tranquillisers or sleeping pills
These use of tranquillisers and sleeping pills relax the muscles in your throat, which can worsen obstructive sleep apnea.
|
Related diseases
|
Impacts
|
| Hypertension1 | 30% of hypertensive people have OSA and 50% of people suffering from OSA have hypertension. |
| Cardiovascular disease, Stroke2 | OSA can lead to Arrhythmia and slower heartbeat; It also associates with an increased risk of stroke. |
| Heart failure3 | Doubled the risk of having heart attack. 70% of coronary artery disease’s patients were found to have sleep apnea. |
| Type 2 diabetes4 | 40% of people with OSA have type 2 diabetes as confirmed by medical research. |
| Alzheimer’s disease5 | Disruptions of sleep architecture and intermittent hypoxia increase the risk of Alzheimer’s disease. |
| Erectile dysfunction6 | The prevalence of Erectile Dysfunction was 51% in male patients with OSA. |
| Mood disorder7 | OSA patients are more likely to suffer from mood or anxiety disorders, PTSD, schizophrenia and dementia. |
| Gout8 | OSA patients had a 50% higher risk of gout compared with individuals who were at high risk of developing gout. |
| Glaucoma9 | OSA patients bear approximately 50% higher risk of having Glaucoma. |
| Periodontitis10 | Studies identified association between periodontitis and OSA and this association was more frequent in women. |
Reference
(2) Patient information series – Seep Mini series #4, Obstructive sleep apnea and heart disease, American Thoracic society.
(3) Marin, J.M., Carrizo, S.J., Vicente, E., & Agusti, A.G. (2005). Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study The Lance, 365(9464), 1046-53.
(4) Einhorn et al. Prevalence of sleep apnea in a Population of Adults With Type 2 Diabetes Mellitus. Endocr. Pract. 2007; 13(4): 355- 362.
(5) Andreia Andrade, Omonigho M.Bubu, Andrew W.Varga, and Ricardo S.Osorio (2018) The Relationship between Obstructive Sleep Apnea and Alzheimer’s Disease
(6) Yiwei Gu, ChangJing Wu, Feng Qin and Jiuhong Yuan. (2022) Erectile Dysfunction and Obstructive Sleep Apnea: A Review
(7) Sharafkhaneh A; Giray N; Richardson P et al. Association of psychiatric disorders and sleep apnea in a large cohort. SLEEP 2005;28(11):1405-1411.
(8) Yuqing Zhang, DSc, Christine E. Peloquin, MPH, Maureen Dubreuil, MD, Edward Roddy, DM, FRCP, Na Lu, MPH, Tuhina Neogi, MD, PhD, FRCPC, and Hyon K. Choi, MD, DrPH (2015) Sleep Apnea and the Risk of Incident Gout
(9) Associations of sleep apnoea with glaucoma and age-related macular degeneration: an analysis in the United Kingdom Biobank and the Canadian Longitudinal Study on Aging. BMC Medicine (2021) 19:104.
(10) Catalina Latorre, Francina Escobar, Juliana Velosa, Daniela Rubiano, Patricia Hidalgo-Martinez, and Liliana Otero (2018) Association between obstructive sleep apnea and comorbidities with periodontal disease in adults